By Kat Henness.
Kat has been a passionate member of the piercing industry for half a decade, and has contributed to education through social media, blog posts, essays, videos and through teaching at UKAPP conferences since 2021. Kat also holds a Masters degree in Microbiology and Immunology from Russel Group university, the University of Nottingham. They have worked in the QMC Medical School, working closely with laboratories performing research on pharmacology, Alzheimers, and human anatomy.
When clients follow appropriate aftercare advice, and given that there are no confounding variables like immune deficiencies or chronic health conditions, healing a piercing is quite straightforward. A common question we all hear as piercing professionals, however, is ‘Wait – How long did you just say my earlobe would take to heal?!’
The easiest way to dispel 3 week healing time myths, and to have a strong grasp on what you are doing as a professional, is to go into scientific detail on the process of wound healing.
The skin and underlying tissue is a complex net of cells all working together to provide protection, structure and nutrients to the surrounding area. When damaged by a procedure such as a piercing, it undergoes three sequential yet overlapping stages of healing. Our bodies are fantastic healers, and when these stages are allowed to happen as normal we can be healing piercings with little to no problem.
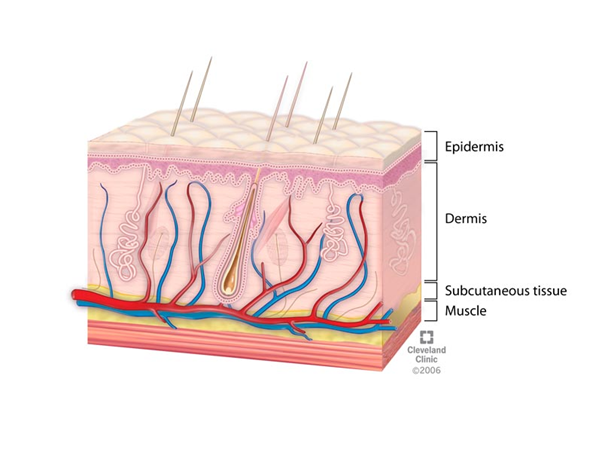
But first, a short anatomy lesson. Body piercings usually pass through the epidermis, dermis, subcutaneous tissue, and cartilage (depending on the placement). The skin is the largest organ, and acts as a physical barrier between you and your external environment.
The epidermis is the outermost layer, and is mostly dead skin cells that are constantly multiplying underneath the epidermis and are pushed up and out over time until they slough off naturally. The dermis is the layer of connective tissue that lies underneath, and functions to support the epidermis. This is where you find extracellular matrix proteins such as collagen, elastin, and other proteins that we will touch on later on. Finally, the subcutaneous tissue (otherwise known as the hypodermis), is the last layer that we pierce through. This fatty deposit is mainly for insulation, but is also filled with tiny blood vessels called capillaries that feed the dermis with nutrients and oxygen.
The cartilage most commonly encountered in the piercing industry is Elastic cartilage, which provides the structural basis of the external ear or Pinna. Elastic cartilage has a minimal blood supply, and is formed from a firm but flexible extracellular matrix of elastin, collagen and specialised cells named Chondrocytes.
Phase 0 – Haemostasis
Before we can consider the three main phases of wound healing, the body has to deal with the more pressing concern of stopping any bleeding. Haemostasis simply means restoring normal blood movement within the blood vessels by causing the blood to clot, preventing major blood loss after any vascular injury.
Blood haemostasis is a very complex cascade of actions working in opposition to one another. On one hand, you have prothrombotic processes which work to cause blood to clot. This is great when you’re bleeding out, but less great when you’re having a stroke. On the other hand, you have anticoagulant processes which work to maintain blood function and liquid consistency.
There are five main named components to haemostasis: Blood vessels, platelets, coagulation promoters, coagulation inhibitors, and the process of clot dissolution.
Immediately after piercing, the walls of the blood vessel will constrict to slow down the flow of blood in the locality of the piercing. Due to the tissue damage, your blood will come into contact with collagen and tissue factors, which promote the activation of platelets. When platelets in the blood come into contact with oxygen, they activate the Coagulation Cascade. The CC is the fastest healing response in nature, and is co-ordinated by enzymes that convert the inactive forms of Prothrombin and Fibrinogen into the activated forms Thrombin and Fibrin. Thrombin and Fibrin work to form a net-like structure that allows platelets to aggregate and plug the damaged blood vessel.
The most common issue with this stage is the introduction of alcohol, which can lower blood levels of Fibrinogen and prevent the coagulation cascade. This is why clients who drink regularly, or attend a piercing appointment drunk, may bleed more and bleed for longer.
Phase 1 – The Inflammatory Phase.
Inflammation is the first phase of healing. It is technically made up of two separate stages that work side-by-side, and begins almost immediately after your piercing. Inflammation can last between 10-14 days.
Inflammation is triggered by both nervous and chemical pathways. Stimulation of the peripheral nerves during piercing allows them to release specific neuropeptides (proteins specific to the nervous system) into the tissue surrounding your new piercing. The most important neuropeptide is Substance P (SP), which binds to Mast Cells and other somatic endothelial cells such as the cells that form your blood vessels.
These neuropeptides have three main targets of action. First, they act on your blood vessels to dilate them and facilitate better blood flow. The more blood that can reach the area of the piercing, the more immune cells, nutrients and oxygenated red blood cells can feed the body’s response.
Second, they target the cells in your blood capillary walls to make them more permeable – this lets important things like water and immune cells enter the area around the piercing more easily. This extracellular space around the piercing is key, as it may have contaminants or bacteria in it. Flooding the area with fluid and immune cells will both dilute any pathogens, and give the immune cells more space to work.
Thirdly, they stimulate your Mast Cells to degranulate. Mast cells are immune cells that live in your connective tissue and are full of important chemicals like histamines and enzymes. When they are stimulated to ‘degranulate,’ they release all of these chemicals into their surrounding area to facilitate swelling and to attract other immune cells to the area from your bloodstream. The two main immune cells in the primary immune response are Macrophages and Neutrophils. Macrophages are tissue-resident cells that consume debris and pathogens whilst releasing cytokines to orchestrate the following immune response. Neutrophils have a similar job, but are short-lived, mobile, and move throughout the lymphatic system to wherever they are needed.
In addition to the nervous system, the damaged cells produced by the action of piercing will release their own chemical signals that are known as Damage-Associated Molecular Pathways (DAMPs). DAMPs consist of a wide range of proteins and lipids that your immune system can bind to, such as fragments of cell membrane, intracellular fluid, and other parts of the damaged cell that should not be present in the extracellular space. These DAMPs are picked up by receptors on the surface of primary immune cells like skin-resident macrophages and localised neutrophils, which follow the trail of signaling molecules back to the source and begin the process of clearing the debris and releasing their own signaling molecules and pro-inflammatory cytokines.

This triple helix project perfectly displays the inflammatory phase. This photo was taken about 30 minutes after piercing, and you can see mild redness and swelling beginning to form.
All of these things work together to bring about inflammation! “Inflammation” is thrown around as a scary word, but it is really important to the healing process! Without it, your immune cells wouldn’t be able to access the piercing site as quickly and the whole healing process would be slowed down. This is why we pierce with slightly longer shafts- To allow for this important inflammation.
Inflammation should not be a chronic condition – The body has tightly regulated mechanisms to resolve inflammation before it can cause damage to healthy cells. This inflammatory resolution is mainly regulated by the balance of two immune cells, the Macrophages and Neutrophils. As previously mentioned, macrophages are tissue-resident cells meaning they are present throughout the body. Neutrophils are mobile, and are attracted to the source of damage. When neutrophils are no longer required at the piercing, they undergo a self-destructive action called Apoptosis and die. Macrophages present in the area will begin to clear away the dead neutrophils. As macrophages phagocytose the neutrophils, they switch from a pro-inflammatory to an anti-inflammatory action which discourages more neutrophils from moving into the area. Over time, the pro-inflammatory cytokines are cleared and the tissue can go back to normal homeostasis. The inflammatory phase concludes.
It is important to note here that the inflammatory phase can be reactivated at any time during the healing process! Any damage to the piercing, or introduction of debris or bacteria, can trigger local macrophages to begin secreting pro-inflammatory cytokines all over again.
Phase 2- The Proliferative Phase
The proliferative phase is the second thing that happens to a new healing piercing. This phase starts after about two days and lasts about 4-6 weeks. Proliferation is the phase in which the piercing truly begins to ‘heal.’ It has three parts.
First, Fibroplasia begins. This simply means that Fibroblast cells found living in your connective tissue begin to work on the piercing site to produce a secure structure on which new cells can grow. Fibroblasts produce type III collagen, which is woven into a new matrix that supports the healing wound. This collagen is formed into loose, messy tangles which are not well-organised and have little structural integrity. This is what makes healing piercings so delicate and more prone to damage.
While this is happening, re-epithelialisation occurs and new skin cells begin to grow on the collagen matrix to surround and protect the fistula (internal hole) of the piercing.
As well as this, angiogenesis begins- This means that new blood vessels are grown to feed the cells working on healing the piercing. This is triggered by skin cells sensing the lack of oxygen surrounding them due to the minor damage to blood capillaries, which then release specific angiogenic growth factors to stimulate new blood vessel growth. Without this process, your piercing would be starved of oxygen and nutrients and would not heal very well. It’s important to note that cartilaginous piercings have naturally low bloodflow, which is a main reason why they are much slower healers than other areas of the body.

This photo was taken immediately after piercing, and you can see we have given this client plenty of space to swell and heal properly without complications. You can’t easily heal a piercing with such a long labret though, which is why downsizing is so important!

Here you can see the same piercing downsized after 4 weeks. A snug fit reduces snags and knocks, and can be more comfortably slept on to avoid bumps. This is the best thing for a healing piercing!
This phase takes 4-6 weeks, and at the end of it the piercing has a fragile seal of new skin running through it. At this time, swelling has gone down and the jewellery may need a downsize. Piercers can gently exchange your jewellery for shorter ones, but clients are definitely not healed enough to start changing the jewellery yourself! This is why any studio which claims to be able to produce healed piercings in 3 weeks is not telling the truth- Biologically speaking, they’re promising the impossible! We haven’t even gotten to the third and final stage of healing yet.
Phase 3- The Remodelling Phase
The third and final phase of healing is the remodelling phase, in which the fresh and fragile fistula is gradually remodelled into a sturdy piercing with functionally ‘normal’ tissue surrounding it. This phase starts at 4-6 weeks post-piercing and can last up to 2 years!
In this phase, the tissue of the piercing channel is slowly changed from fragile nets of collagen matrices to fully functioning normal tissue, with its own blood supply, nerves, epithelial tissue and dermal layer. During this time the piercing will slowly settle down into a comfortable, boring piercing which feels like the client has had it forever!
The four main stages of remodelling include collagen remodelling, wound contraction, tissue maturation and finally scar formation. All piercings are technically scars.
The loose, messy nets of type III collagen are slowly reformed into type I collagen by myofibroblasts. Type 1 Collagen is slower to form and more energy-intensive to produce, but its uniform structure gives it a much higher tensile strength. This makes the piercing more robust. That being said, scar tissue can never be as strong as normal skin, and in fact has about 20% less tensile strength. Piercings will always be slightly more fragile, but this can be corrected for with lifestyle and behavioural changes from the client.
Wound contraction is an interesting part of the remodelling process. Wounds contract in order to decrease the amount of connective tissue the body needs to build in order to fill the wound bed. You can often see soft-tissue piercings contracting over time – This is what gives them that dimpled effect.
Finally, scar maturation will occur over the following 8-12 months. Healed but immature piercings will often appear slightly red, or raised. This is because of excess collagen deposition and increased vascularity during the healing process. Over time the extra blood vessels will shrink, and the scar will pale and flatten.
Educated piercers will state that it takes between 6 and 12 months for a full heal on any piercing, and this is why – You’ve given it time to settle and become more robust. However if you think of a healing piercing at 6 months old, and then compare it to a piercing you’ve had for over 2 years, you can still notice a difference! The 6 month old piercing may still have some redness and some discomfort when it is manipulated and it may be more prone to irritation than a really mature piercing. A 2+ year old piercing is mature and durable, and so should have no redness, swelling, discomfort- It will just feel like normal skin. This is what we all aim for with our piercings and this is what can be achieved with proper aftercare following a good piercing.

This conch piercing is a perfect example of a well-healed and mature piercing! You can see no redness, puffiness or swelling. It just looks like skin.
References:
Cañedo-Dorantes, L. and Cañedo-Ayala, M. (2019). Skin Acute Wound Healing: A Comprehensive Review. International Journal of Inflammation, [online] 2019, pp.1–15. Available at: https://www.hindawi.com/journals/iji/2019/3706315/ [Accessed 20 Feb. 2021].
Enoch, S. and Leaper, D.J., 2005. Basic science of wound healing. Surgery (Oxford), 23(2), pp.37-42.
Zaidi, A. and Green, L., 2022. Physiology of haemostasis. Anaesthesia & Intensive Care Medicine, 23(2), pp.111-117.
Almadani, Y.H., Vorstenbosch, J., Davison, P.G. and Murphy, A.M., 2021, August. Wound healing: a comprehensive review. In Seminars in plastic surgery (Vol. 35, No. 03, pp. 141-144). Thieme Medical Publishers, Inc..
Zeng, J., Pan, Y., Chaker, S.C., Torres-Guzman, R., Lineaweaver, W.C. and Qi, F., 2024. Neural and inflammatory interactions in wound healing. Annals of Plastic Surgery, 93(2S), pp.S91-S97.
Suvas, S., 2017. Role of substance P neuropeptide in inflammation, wound healing, and tissue homeostasis. The Journal of Immunology, 199(5), pp.1543-1552.
** Raziyeva, K., Kim, Y., Zharkinbekov, Z., Kassymbek, K., Jimi, S. and Saparov, A., 2021. Immunology of acute and chronic wound healing. Biomolecules, 11(5), p.700.
Sophia Fox, Alice J et al. “The basic science of articular cartilage: structure, composition, and function.” Sports health vol. 1,6 (2009): 461-8. doi:10.1177/1941738109350438
Ortega-Gómez, Almudena et al. “Resolution of inflammation: an integrated view.” EMBO molecular medicine vol. 5,5 (2013): 661-74. doi:10.1002/emmm.201202382